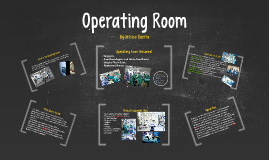
Operating Room
Transcript: Operating Room Nurse Late 1800s-1900s Although there is evidence of surgery taking place back in prehistoric times, the late 1800s is when it became noticeably more advanced. Medical developments like anesthesia, antibiotics, and antisepsis made surgery a more popular, safe, and a beneficial option for patients. This is when perioperative nursing really started to develop, because there was a need for qualified professionals to assist the surgeon, and most believed that this was the nurse’s role. Perioperative nursing was considered very prestigious around the time of the 1880s, and the operating room nurse’s salary was higher than that of what was called a “general duty nurse.” These nurse’s responsibilities ranged from sterilization of the instruments to assisting the surgeons in general. 1940s-1950s One of the main responsibilities of the operating nurse at this time was still the sterilization of instruments by washing them by hand, assembling them in appropriate sets, and sterilized them in what was called Bard Parker solution, which was a combination of formaldehyde and alcohol. It was also the nurse’s responsibility to wash, dry, and inspect the gloves that were used, because there were not any disposable gloves. OR nurses were also responsible for “recovering” their own patients, because there were no recovery areas at this time. Throughout this time period the operating room nurse’s role was beginning to be viewed as a technical one instead of a caring role. Because of this, some felt as though this specialty lost some of its prestige. The Association of Perioperative Registered Nurses (AORN) formed in 1954 1960-1980 The debate about whether or not perioperative nursing was just a technical skill intensified even more in the 1960s. Many people believed that the technicality of operating room nursing was not compatible with the caring aspect of nursing. In the early 1960s people also started to consider the operating room nurse as just the “handmaiden” of the surgeon. Because of this, perioperative nursing was less respected. In the late 1960s, the operating room nurse’s training centered mainly on technical skills, which made even more people believe that it was technical trade rather than a nursing specialty. Also, this time period is when operating room nursing was removed from the academic curriculum of most nursing schools. Therefore, students were not exposed to operating room nursing, and were less likely to choose this specialty upon graduating. Hospitals then had to create their own operating room training programs, but many were not taught using holistic practice based on nursing theory. This also furthered the belief that perioperative nursing was a technical trade. The Standards for Administrative and Clinical Practice in the Operating Room, now called Perioperative Standards and Recommended Practices, was published in 1965 by the Association of Perioperative Registered Nurses (AORN) 1980-2000 During this time period is when hospitals really began to hire more operating room nurses with a BSN. There were still misunderstandings about what perioperative nurses did, and there was another debate that began about replacing operating room nurses altogether with other less trained and less expensive technicians. 2000-2010 There has been an ongoing debate over whether perioperative nursing should be considered a technical skill or “real” nursing since it became a specialty. This type of nursing is still evolving because of the constant developments in surgical technology. Throughout the 21st century so far the perioperative nursing specialty has been facing major recruitment and retention issues. Today many operating room nurses have heavy workloads, high patient acuity, and staffing shortages. The perioperative nurse specialty is facing some difficulties and there is a great need to make nurses, nursing students, and society in general, understand that this nursing specialty is important and needed because nurses are considered to be the most qualified professionals who can assist with surgery and be the best patient advocates. Many operations were performed in private homes. Wooden furniture, walls, floors and seating capacity for the medical audience in typical hospital operating rooms were seen as creating unclean conditions. •Early recognition of the importance of hand washing. •Gradually, cloths, instruments and dressings were meticulously cleaned. •The practice of asepsis was advanced. •Due to the Influence of Louis Pasteur, Various Types of Sterilizers Were Developed and Asepsis Became the Standard •Rubber gloves were introduced and later the face mask was adopted •The student nurse was responsible for sterility of equipment. •She prepared the room, scrubbed the floor and walls with antiseptics. •Dressings were boiled, soaked and wrapped in antiseptic towels or large glass jars. •She prepared everything that was needed including: •Hot water bottle •Stimulants •Clean towels •Soft rags