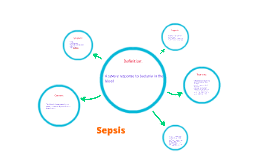
Sepsis
Transcript: Stage II: Sepsis Infection accompanied by an acute inflammatory reaction with systemic manifestation associated with endogenous mediators Macrophage and Neutrophils release cytokine in to circulation to improve local response Leads to recruitment of macrophages and platelets Acute phase sepsis decrease pro inflammatory mediators by the release of endogenous antagonist Maintenance of any tubes and drains. - Check placement, patency, and output/input Ventilator care -Frequent assessments and monitoring Prophylactic care -Pressure ulcers and deep vein thrombosis Two or more of the following Temperature of > 38 C or < 36 C Heart Rate of > 90 Respiratory Rate of > 20 WBC count > 12 x 10 / L Andrew, Jimmy, Kara, Ryan, and Kat Systemic inflammatory response syndrome (SIRS) Sepsis summed up is: Sepsis associated with organ dysfunction, hypoperfusion, or hypotension. Examples: Signs of kidney hypoperfusion: oliguria Signs of brain hypoperfusion: ALOC Genitourinary The renal system is extremely sensitive to ischemic-perfusion injury; hypoperfusion can lead to Acute Renal Failure Oliguria Anuria Elevated Creatinine Metabolic Acidosis Increased Lactate Decreased Lactate Clearance Acute Tubular Necrosis A systemic inflammatory response in the presence of an infection... Pathophysiology Pathophysiology Stress ulcer prophylaxis: using histamine antagonists blockers or proton pump inhibitors. DVT prophylaxis Improve patients overall nutritional status, enhance immune function, and promote wound healing = daily caloric intake of 25 – 30 kcal/kg of usual body weight. Enteral route preferred. Management and treatment of specific organ failure. Stage I: SIRS Fibrin Deposition Platelet aggregation Coagulopathies Leukocyte liposomal Activation of pathway to increase inflammation by recruitment of neutrophils and monocytes. The inflammation to the endotoxin that Gram – negative bacteria release activates cytokine. Infection Finding and eradicating the cause of infection At least 2 blood culture plus urine, sputum, and wound culture Antibiotic therapy started within 1 hr of recognition Specific source of infection should be established within 6 hours. Sepsis induced multiple organ failure or a clinical determination of high risk for death = administration of recombinant human activated protein C or Xigris (drotrecogin alfa [activated]) IV at an infusion rate of 24 mcg/kg/hr for duration of 96 hours. Pathophysiology Hepatic Posttraumatic Hepatic Insufficiency Jaundice (Hyperbilirubinemia) Increased Liver Enzymes (AST and ALT) Decreased Albumin Gastrointestinal Bacterial Translocation Endogenous Endotoxemia Low perfusion or hypoxia can cause ischemic necrosis of the GI tract Ronga Stage III: Severe Sepsis Sepsis associated with organ dysfunction, hypoperfusion, hypotension 3 conditions: known or suspected infection, two or more clinical indications of systemic inflammatory response, and evidence of at least one organ dysfunction 2 most common organs to demonstrate dysfunction are cardiovascular and system and lungs Persistent hypotension requiring vasopressors: cardiovascular compromise Pulmonary dysfunction is manifested by PaO2/FIO2 ratio less than 300, indicated ALIPerfusion abnormalities such as lactic acidosis Two or more of the following Temperature of > 38 C or < 36 C Heart Rate of > 90 Respiratory Rate of > 20 WBC count > 12 x 10 / L Increase cellular oxygen supply & decrease cellular oxygen demand. Fluid resuscitation: increase intravascular volume and increase preload for CVP of 8-12 mm Hg. (Crystalloids of colloids) Fluid Challenge for hypovolemia with at least 1000 mL crytalloids or 300-500 mL of colloids over 30 minutes. Vasopressor administration: maintain a MAP of at least 65 mm Hg First choice agents: Norepinephrine or dopamine Alternate choice: Epinephrine Identifying Patients at Risk MODS results from progressive physiologic failure of two or more separate organ systems. It is defined as the “presence of altered organ function in an acutely ill patient such that homeostasis cannot be maintained without intervention” To understand MODS, you must first understand the continuum of sepsis. Extremes of age (<1 and > 65 years) Surgical/invasive procedures Malnutrition Patients on broad spectrum antibiotics Chronic illness/multiple co-morbidities Compromised immune status Malignancies Use of transplant/immunosuppressant drugs Increase in # of drug-resistant organisms SIRS with a present infection At-Risk Populations SIRS Systemic inflammatory response to a variety of severe clinical insults, manifested by two or more of the following conditions: Temperature >38 C or <36 C Heart rate >90 beats/min Respiratory rate >20 breaths/min or PaCO2 <32 mm Hg White blood cell count >12,000/mm3, <4000/mm3, or >10% immature band forms What is it?? Goal Directed Management Respiratory/Pulmonary The most commonly affected organs are the lungs, seen manifested as ALI and ARDS Patients with lung dysfunction are more critical Tachypnea with